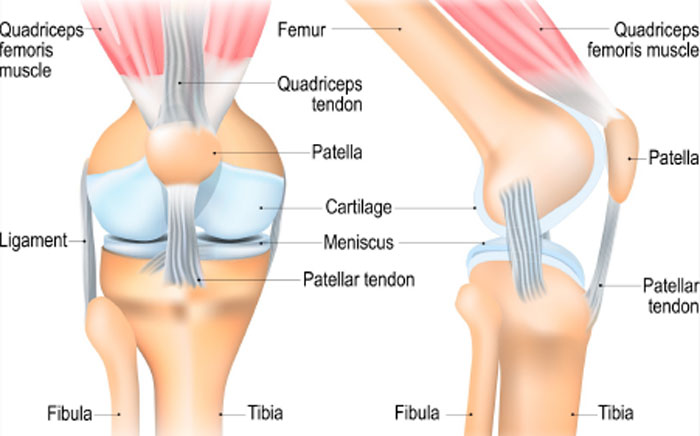
What is the MPFL?
The medial patellofemoral ligament is a band of tissue that acts like a ‘seat-belt’ to stabilise the kneecap as you start to bend the knee. It is inside the knee so you can’t feel it when you press around the knee. As you bend and straighten the knee the kneecap glides along the groove on the front of the thighbone and the MPFL moves with it like a ‘windscreen-wiper’ keeping it in the groove.
The MPFL attaches the inside part of the kneecap to the thighbone (femur). It helps the kneecap to track properly in the groove on the front of your thighbone and stabilises the kneecap during movement.
What happens to the MPFL when the kneecap dislocates?
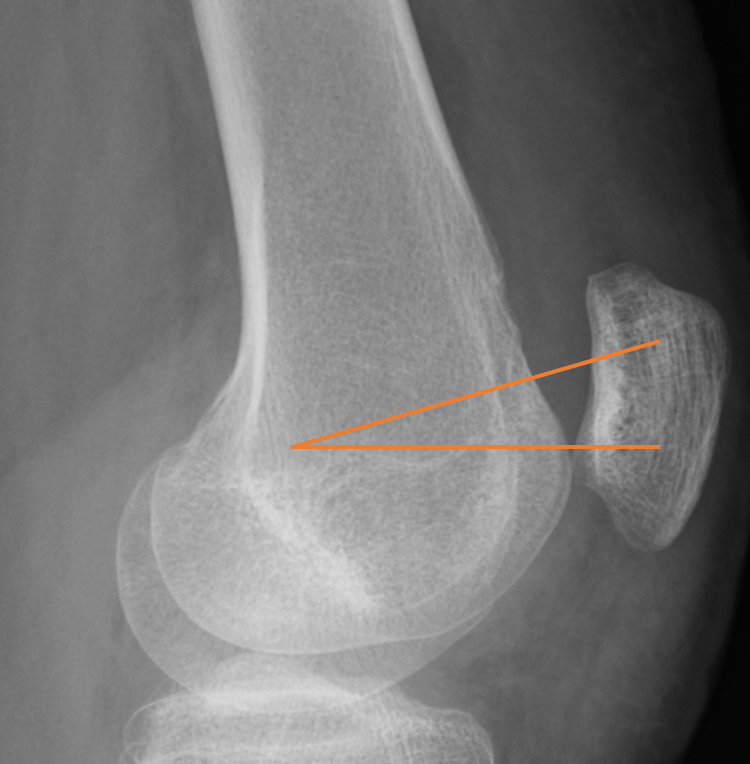
When the kneecap dislocates it jumps sideways out of the groove and the soft tissues around the kneecap are stretched and can tear. In about 87-100% of dislocations the MPFL ruptures.
Does the MPFL heal once it has ruptured?
If left untreated the stretched or torn MPFL can heal but as it is stretched it does not provide the tight seat-belt effect on your kneecap.
A bit like getting into a car and leaving your seat-belt really loose or not doing it up, the seat-belt then won’t work properly and you will move about if you have a car crash.

When do you reconstruct the MPFL?
With a torn or stretched MPFL the kneecap is at greater risk of dislocating again which can in turn cause damage to the cartilage on the surface of the kneecap.
Other factors such as the shape of the groove the kneecap sits in, the shape of your thigh bones and the position of your kneecap can also increase the risk of you dislocating again.
If the kneecap has become unstable (such as more than 4 dislocations) or feels very wobbly day to day then we would have a discussion as to whether the operation is appropriate for you.
What is an MPFL reconstruction?
This operation is a day case which means you come in on the day and usually go home on the same day. It involves having an anaesthetic to put you to sleep and sometimes a nerve block to help numb the area for pain relief.
One of your tendons that you don’t need (the gracilis tendon) is most commonly used. It is detached from where it sits on the inside of your knee and attached to your kneecap using anchors. It is then tensioned and attached to your thigh bone to reproduce your torn MPFL.
Sometimes we use a donor tendon (allograft) if your own tendons are not suitable. These a tendons harvested from donors which have been treated and screened for infections.
More information can be found here:


What are the risks of an MPFL reconstruction?
You will have some scars around the knee and some people find they have a numb patch of skin around the scar after surgery which may be permanent.
Do you do any other operations at the same time?
I will have a look inside your knee (arthoscopy) to check the cartilage lining of your knee joint and make sure there is no other damage.
Depending on the shape and position of the kneecap on the imaging investigations such as MRI, additional procedures are sometimes needed. Sometimes the MPFL reconstruction is done in combination with other procedures such as a tibial tubercle osteotomy (to move the kneecap down and across into the groove), trochleoplasty (to deepen the groove) or distal femoral osteotomy (to straighten out the thigh bone). Where possible all the operations are done at one sitting.
What happens after the surgery?
If the operation is an isolated MPFL reconstruction you are walking unrestricted straight away, with crutches to help you walk full weight bearing. You keep the wound dry for 2 weeks then start physiotherapy. The physiotherapist will help build up your strength and work on improving how you use your knee to try to reduce the risk of further injury.
When can I drive?
By 6 weeks you should be back to driving.
When can I go back to sports?
Your physiotherapist or personal trainer will work with you to make sure you are fit to go back to sports. Usually this starts with lots of work in the gym before you can go back to contact sports such as netball, football etc at about 9 months.
This varies between patients, generally the fitter you are before surgery, the easier it is for you to recover.
Will this operation stop me developing arthritis in later life?
The MPFL reconstruction helps to stabilise the kneecap and hopefully if it stops the kneecap dislocating it will then also help to protect the cartilage. However, there are lots of reasons why people develop arthritis so we cannot guarantee that the operation will reduce your risk.