Why has my kneecap dislocated?
Kneecaps dislocate for lots of reasons. You may have a normal knee and having knocked the side of your kneecap it has dislocated.
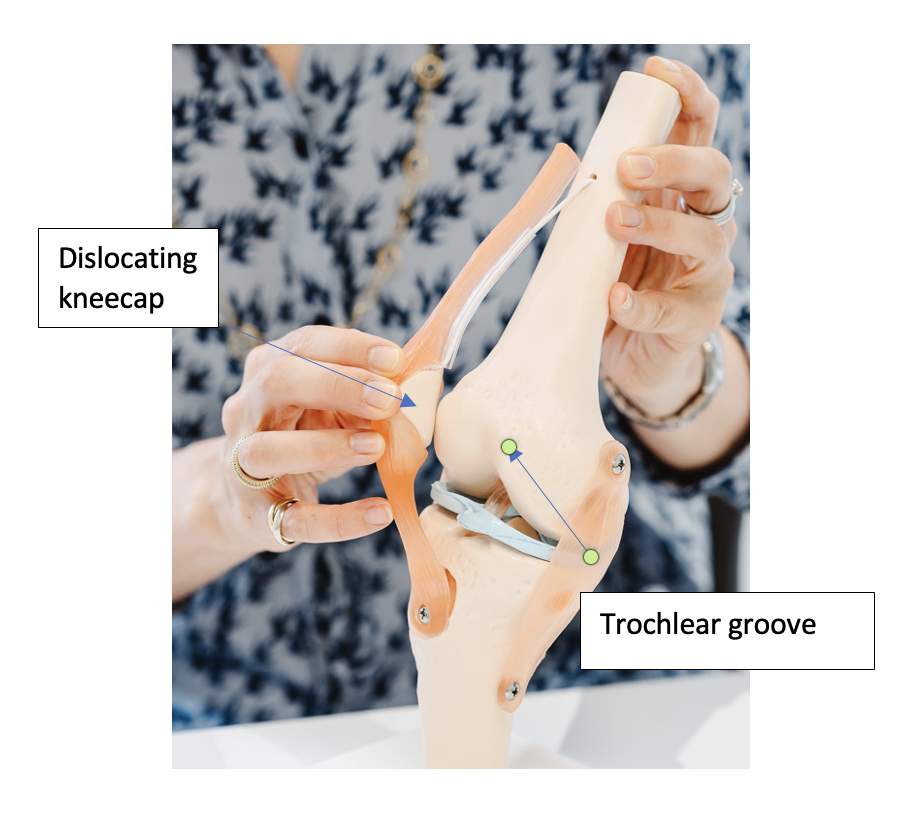
If your kneecap sits in a shallow groove or you have hypermobility this can contribute to your risk of dislocating your kneecap
Will my kneecap dislocate again?
In 15-45% of people after a first dislocation their kneecap dislocates again
Why has my knee swollen after dislocation?
After a dislocation blood collects in the knee causing swelling. This is gradually absorbed by the body after a few weeks.
Have I injured anything else when I dislocated my kneecap?
You can cause damage to the cartilage on your kneecap as you dislocate then as your kneecap relocates. If it is a large piece of cartilage and bone you may need surgery to re- attach it to your kneecap.
With smaller pieces, sometimes they float around the knee and ‘stick down’ on the knee capsule where they do not cause a problem.


What if I’m not sure what I want to do?
You can ask for ‘thinking time’ to consider your treatment options and discuss them with your family. It might be that you want to delay treatment until after school exams or plan for the holidays to give yourself time to recover before going back to school, university or a job.
You might want a second opinion to be sure and I can suggest a colleague to see if you would like to do that. Often with complex cases I will discuss with colleagues in the British Patellofemoral Society as it is safer to make sure that the treatment plan is right for you.
What happens next?
Not all kneecap problems need surgery. I might suggest a course of physiotherapy, fit a brace or injections to help you. I work with a team of physiotherapists and radiologists to ensure your treatment journey suits you and your busy lifestyle.
What if I need surgery?
If you need surgery we would plan a time that is right for you. I will explain what the surgery involves and what the benefits and possible complications are. You can also refer to information on my website about your condition and surgical options.
Before surgery you can improve your fitness by eating healthily and giving up smoking. You may also be seen in the pre-admission clinic for blood tests and to ensure you are fit and ready for surgery.
What’s the difference between health insurance and self-funding?
If you have a health insurance policy, we will give you the procedure codes to ask the insurance company for pre-authorisation. If you are self-funding we will help you liaise with the London Bridge or Portland Hospital to get an idea of the costs of the treatment package.
What do I need to prepare on the day of admission?
We will contact you before your surgery explaining where you need to go (London Bridge Hospital or the Portland Hospital) and what time you need to come in. You will also be told when to stop eating and drinking. Usually you stop eating about 6 hours before your surgery and you can have water until 2 hours before your surgery. We will also give you an idea as to how long you will be in hospital and how much time you need to take off work and sports so you can start to plan your life around your recovery.
Should I still take my medicines?
Continue to take your medicines unless you have been told to stop taking them when I see you in clinic. For women on the contraceptive pill we will discuss with you before the surgery whether you should stop taking the pill and use alternative forms of contraception.
Will I need to have stitches removed?
I like to use dissolvable stitches so you don’t have to have stitches taken out. I take pride in neatly closing a wound to ensure you have as neat a scar as possible. We usually organise a wound check two weeks after your surgery to make sure the wound has healed up and also to check on your progress. For the first two weeks after surgery you need to keep the wound dry and protected to help with healing.

What are the treatments for Coronary Artery Disease?
The treatment will be tailored to your needs and can be managed effectively in 3 ways: