What is a kneecap dislocation?
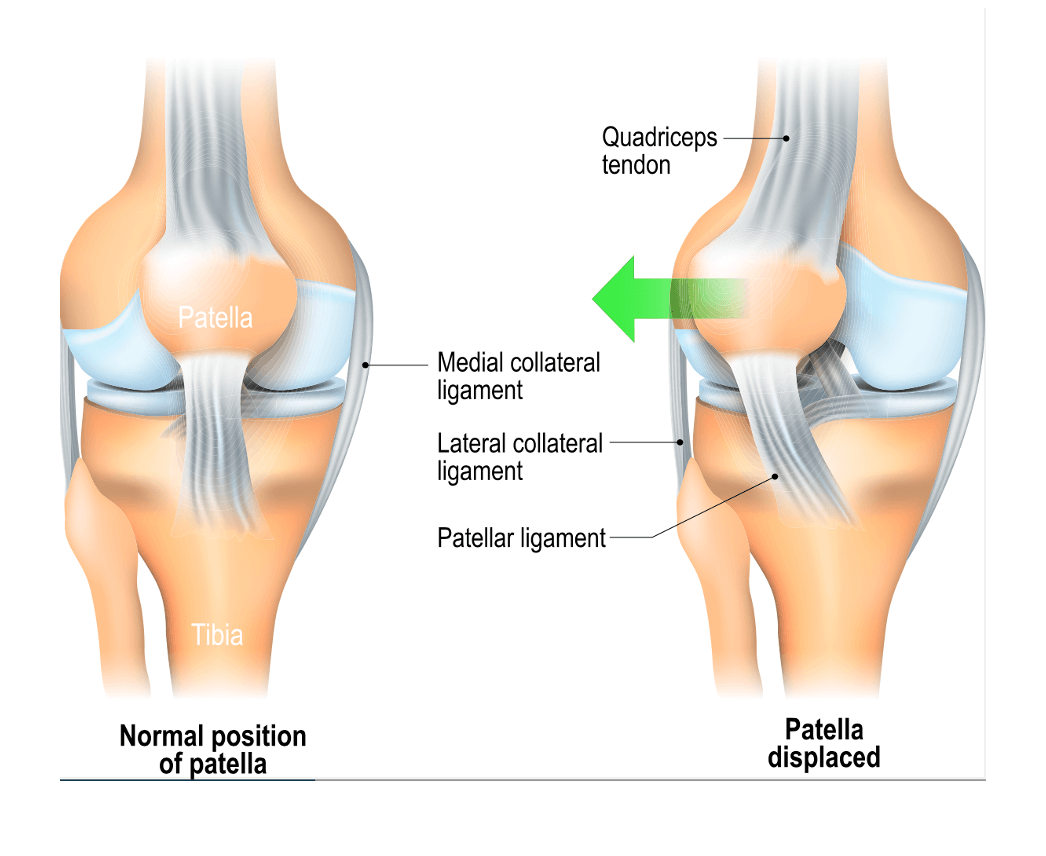
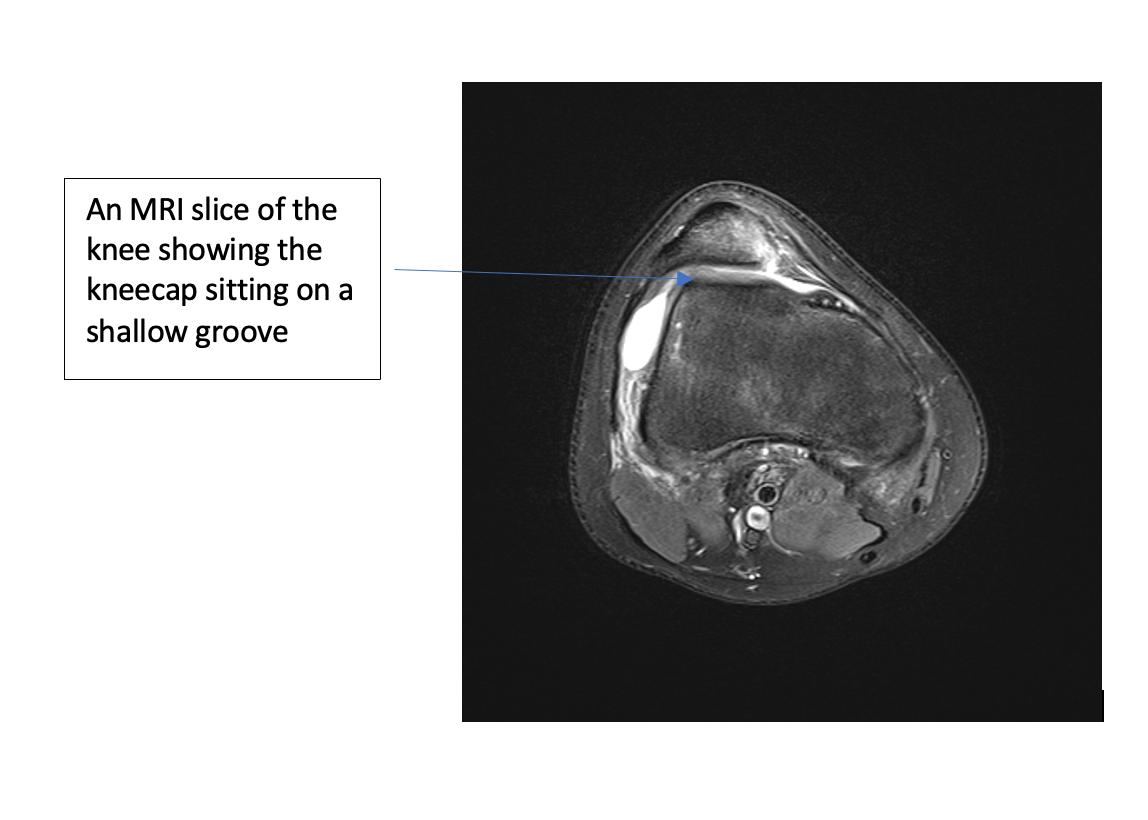
A kneecap dislocation means that the kneecap (patella) has jumped sideways out of its vertical groove (trochlear groove). Dislocations can occur following a fall or twisting injury, or they can occur in people whose anatomy differs slightly to that of the general population e.g. those that have very flexible joints or a very shallow groove.
What happens when I am seen in the hospital emergency department (ED or A&E)?
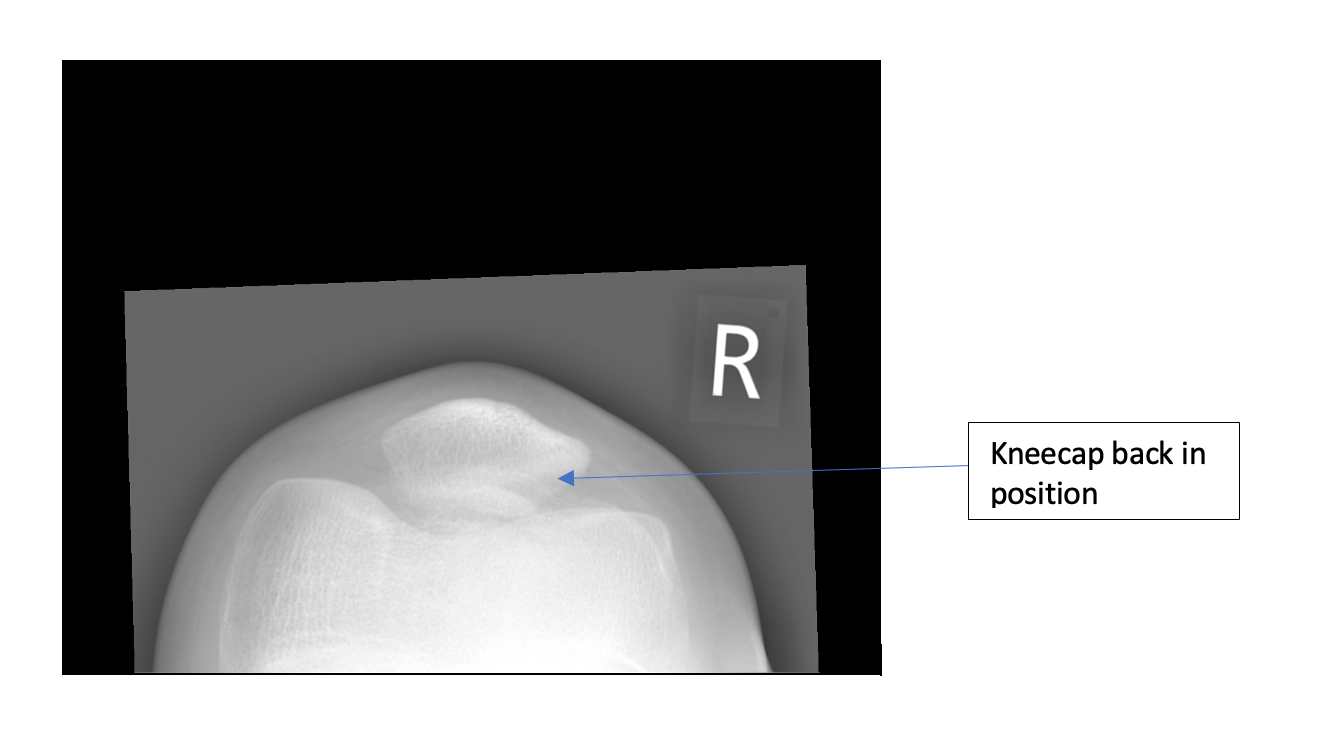
Your kneecap will have either moved back into place of its own accord which can happen if you gently straighten the knee. Sometimes the kneecap is stuck dislocated and the ED doctors will give gas and air, or a light anaesthetic to allow the leg to be straightened and gently push the kneecap back into the groove.
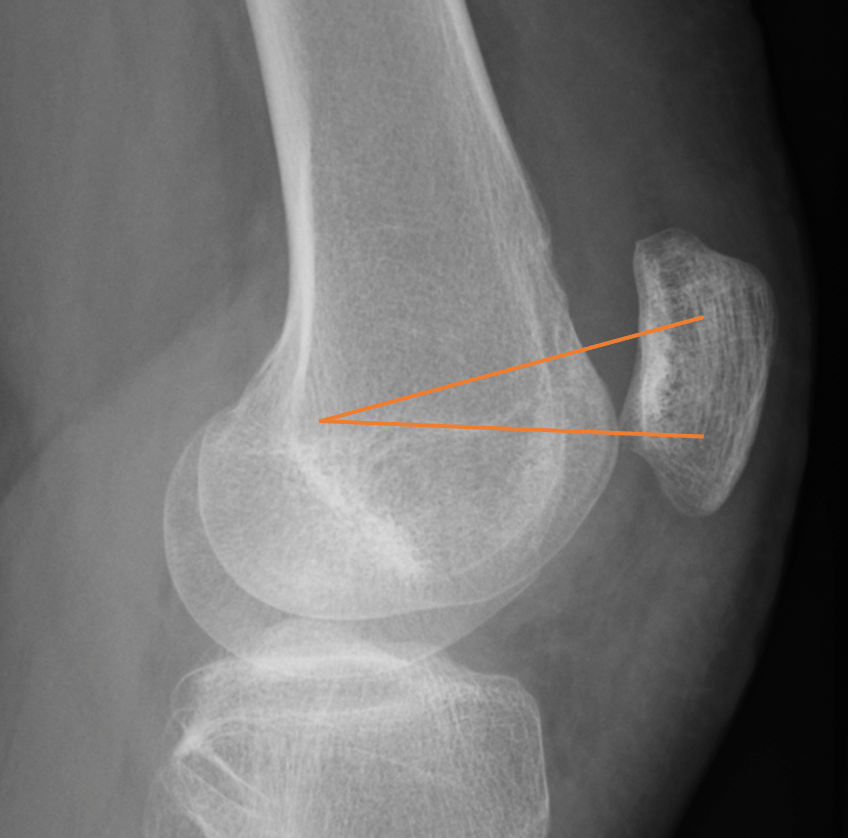
An X-ray (radiograph) is then taken to make sure there are no fractures and that the kneecap is back in the right position.

Often you will have been fitted with a knee brace in A&E which will hold your leg straight. This can be worn as required for 2 weeks, to help with pain and swelling. It can be removed for hygiene purposes (bathing) or if your pain and swelling has settled you can remove it earlier. The knee brace is to help with the pain but can be removed as soon as possible.
It is safe to put your bodyweight through the leg as normal as soon as you feel able. You can use crutches for support, although they are not strictly necessary.
After 2 weeks it is important to gradually stop wearing the brace and get the knee moving in order to begin strengthening the thigh muscles again.
Physiotherapy can start straight away to help reduce the swelling and regain range of motion. Physiotherapy will help to strengthen the muscles around your knee further.
The majority of first-time dislocations will go on to heal by themselves, an MRI scan is performed if indicated to rule out any other injury and give you a prognosis as to whether you are at risk of further dislocations.
How long does it take to heal?
There will have been some ligament and muscle damage caused when your kneecap moved out of place. Healing times are dependent on multiple factors and at this point in time they would be difficult to quote accurately.
Please be aware healing times can vary and may be influenced by factors such as age, pre-existing medical conditions, previous dislocations etc…
When do I need an MRI scan?
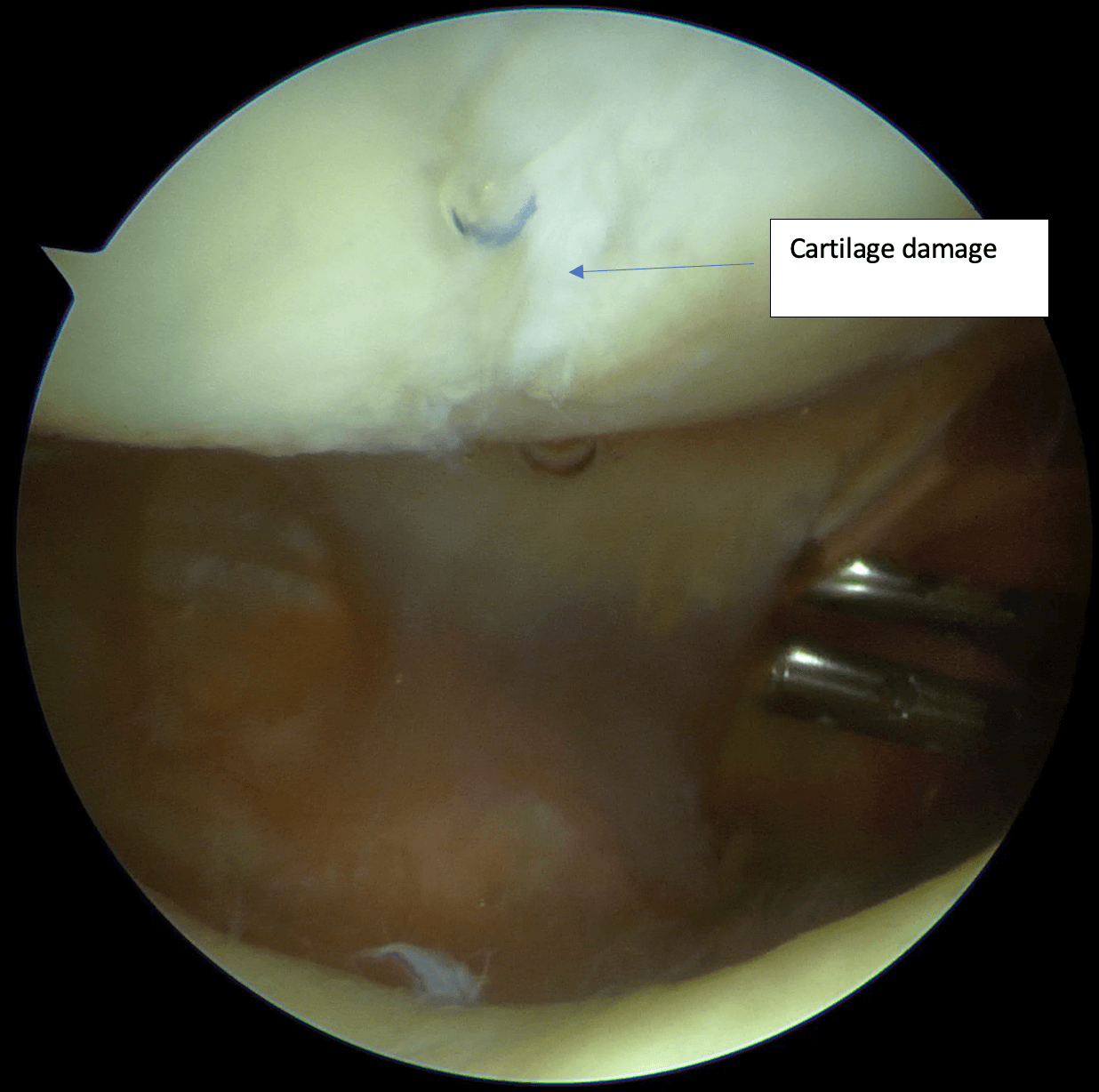
MRI scans are used to assess both bones and soft tissues (such as ligaments and cartilage). They will show the anatomy of your knee in great detail. MRIs do not use radiation and are a relatively safe investigation to undergo. However, some people may not be able to have an MRI scan for various reasons such as having metalwork in their body or being pregnant/breastfeeding. Please see the NHS advice on MRI safety if you are unsure of your eligibility to undergo the scan MRI scan – Who can have one – NHS (www.nhs.uk).
Return to work/Sick certificates
Manual workers If you are unable to undertake “light duties” at work you may need a sick note.
Office based You can return to work when you feel comfortable to do so and so long as duties do not interfere with your recommended treatment plan.
Driving You should not drive when wearing a knee brace. You should only drive once you are pain free and able to perform an emergency stop safely. If you do not have full control of your vehicle, you should not drive.
Holidays If you have a holiday booked a dislocation may count as a ‘pre-existing condition’ and you should check with your holiday insurance to see if this affects your cover.
Some people with a reasonably good deep groove just need a medial patellofemoral ligament (MPFL) reconstruction
This operation involves taking one of your hamstring tendons and attaching it to your kneecap with two small tunnels and anchors in your kneecap and a tunnel in your femur (thigh bone). This is done as a day-case and means you are walking and moving the knee straight away.
If you have a very shallow groove, the surgery aims to deepen the groove by making flaps in the bone of your groove and moving them (a trochleoplasty). They are then held in the new position by dissolvable anchors and tape and you are encouraged to move the knee straight away. This is a larger operation than an MPFL reconstruction and usually due to pain you stay in hospital for a couple of nights but are moving the knee full weight bearing straight away.
If your kneecap is tilted or is positioned very high then a tibial tubercle osteotomy will be used to move it to a better position. The new position is held with some screws and you will be placed in a knee brace to limit your movement for up to 3 months until it has fully healed.

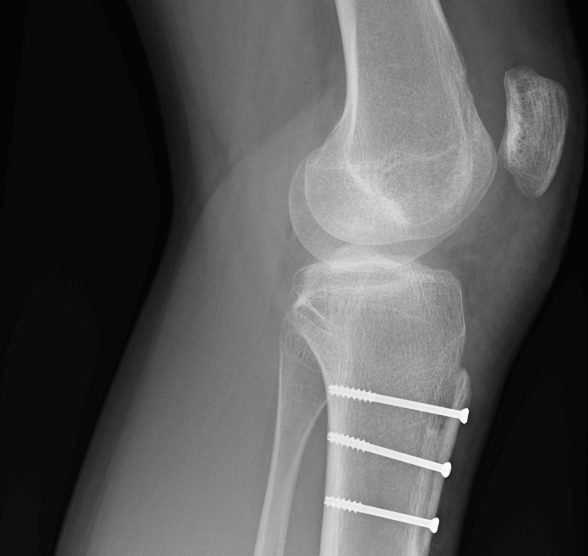
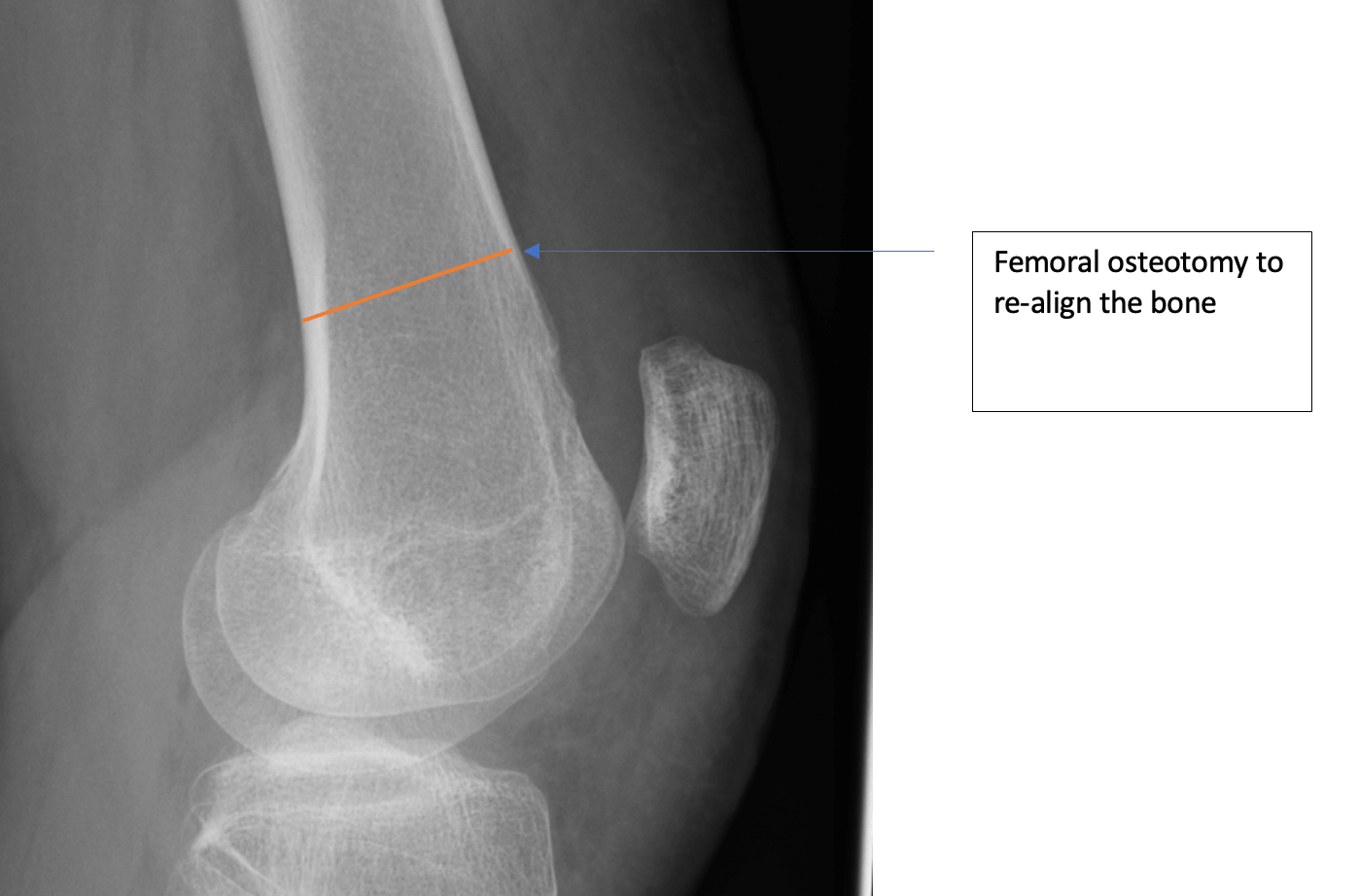
In some cases, when I examine you I may find that your thigh bone is not straight, if this is the case I would ask for a standing X ray to see if you are ‘knock kneed’ or ‘bow legged’ as well as a CT scan to assess the rotation or twist in the thigh bone. If your thigh bone is twisted or bent, we would perform a distal femoral osteotomy to straighten the bone.
How do you decide what surgery is needed?
I would review your MRI, CT and XR with you and explain what the plan is. With more complex cases it is common to discuss your case with other expert colleagues in the field (a multidisciplinary meeting) to ensure we agree what surgery you need.
What if I can’t decide?
If you are not sure you can have time to think about the surgery or you can ask for a second opinion, I work with other experts in the field who I can ask to review your case.